Efficiency
is imperative
Efficiency
is imperative
Future health systems must become more efficient through a system-wide transition to value-based healthcare.
Defining efficiency and value
Health systems are estimated to waste up to 20% of spending on interventions that do not improve health outcomes.
While we support greater investment in health, according to the economy of wellbeing (See Introduction), increased funding should be combined with action to reduce inefficiencies.
Future health systems must become more efficient, but it is important to define efficiency carefully. We believe that improving efficiency means maximising the patient- and population-level health outcomes achieved through a certain health investment, or maintaining the same outcomes while achieving long-term savings for health systems or society. This is closely related to the concept of value-based healthcare.
EFPIA believes that efficiency and value should be defined in people-centred ways, i.e. based on what matters most to patients themselves. This is one of six key principles for value-based healthcare that we share with fellow members of the European Alliance for Value in Health – representing patients, healthcare practitioners, health authorities, healthcare management and the medical technology industry. More traditional ways of defining efficiency in relation to output (e.g. number of procedures performed), ignores the appropriateness and quality of care and the health outcomes achieved for patients.
We need to identify inefficient, low-value spending and redirect these resources to services and technologies known to generate better value. This way, we can improve patients’ health outcomes and quality of care without increasing overall expenditure and realise the full return on investment from health spending.
Six key principles of value-based, sustainable, and people-centred health systems:
1. Outcomes that matter to people and patients, as well as benefits valued by health systems and societies, are at the centre of decision-making
2. Interventions and services addressing prevention, social care and healthcare are organised in an integrated way around people and patients
3. Resources are allocated towards high value care and prevention, with outcomes and costs of care measured holistically
4. Continuous learning, education and healthcare improvement is based on evidence, and supported by data and insights
5. Innovative ways of care delivery are fostered
6. Financing models and payments reward value and outcomes.
Efficiency gains across health systems
Inefficiency and wasteful in healthcare can occur in different forms, for example:
- Some patients receive repeated diagnostic tests or services, simply because information is not shared across providers.
- Some patients receive ‘low-value care’, i.e. care that is ineffective, or that works for only some groups of patients.
- Patients sometimes receive care that causes serious complications that could have been avoided. It is estimated that around 10% of hospital expenditure goes to correcting preventable medical mistakes or hospital-acquired infections.
Improving efficiency and reducing waste is not about cutting costs, but about investing smartly in health systems, as we pointed out in the EFPIA report ‘Strengthening health systems through smart spending’.
Integration
Poor co-ordination between healthcare providers within fragmented health systems is a key source of inefficiency – causing duplication and inconsistent care or poor follow-up. Integrated models that align all resources and incentives toward measurably improving outcomes that matter most to people will be more efficient (See People-Centricity and Outcomes). More integrated budgets spanning the health and social care sectors would encourage strategic investments into services and technologies that free up resources in the longer-term or elsewhere in the system for reinvestment.
Digital health technologies will support these efficiency gains, by helping to measure performance and optimise resource allocation.
Disease prevention
Future health systems must invest more in primary disease prevention and public health. This is one of the most efficient ways to protect people, health systems and economies.
Each year over 1 million premature deaths in the EU – two thirds of the total – could be avoided through better disease prevention and healthcare. Almost two thirds of these avoidable deaths are preventable through effective primary prevention and other public health measures.
Vaccination offers a prime and timely example of disease prevention and high-value innovation can have enormous benefits to health systems and society. Vaccination has been a cornerstone of European public health for decades, preventing disease, reducing the burden on health services and supporting healthy populations. Vaccines are a ‘best buy’ in health, providing a substantial return on investment. Now, COVID-19 has underscored their unparalleled value in protecting people, health services and broader economies.
However, at present only 3% of health spending is devoted to disease prevention and public health across the EU and less than 1% (median 0.3%) to immunisation funding.
Many medicines also play an important role for secondary prevention, especially in chronic diseases such as diabetes and cardiovascular disease, to prevent serious events and complications.
Timely and effective treatment
Investing in better screening and treatment can avoid downstream costs.
The remaining one‑third of the 1 million avoidable deaths in Europe each year could be avoided through earlier and better healthcare.
Most of the healthcare costs of chronic diseases are spent on hospital care for advanced disease and complications. Earlier diagnosis and effective, timely treatment gives far better patient outcomes, avoids unnecessary downstream costs, and reduces the societal life-time burden of ill health. In fact, poor adherence to prescribed medicines is thought to cost as much as EUR 125 billion in avoidable hospitalisations, outpatient visits and emergency care.
For example, diabetes absorbs 9% of the total health expenditure in the EU and is rising. An estimated 75% of this expenditure is for complications that could be significantly reduced by innovative medicines, such as diabetic retinopathy, heart and kidney failure. However, only 6.2% of diabetes expenditure is used for medicines.
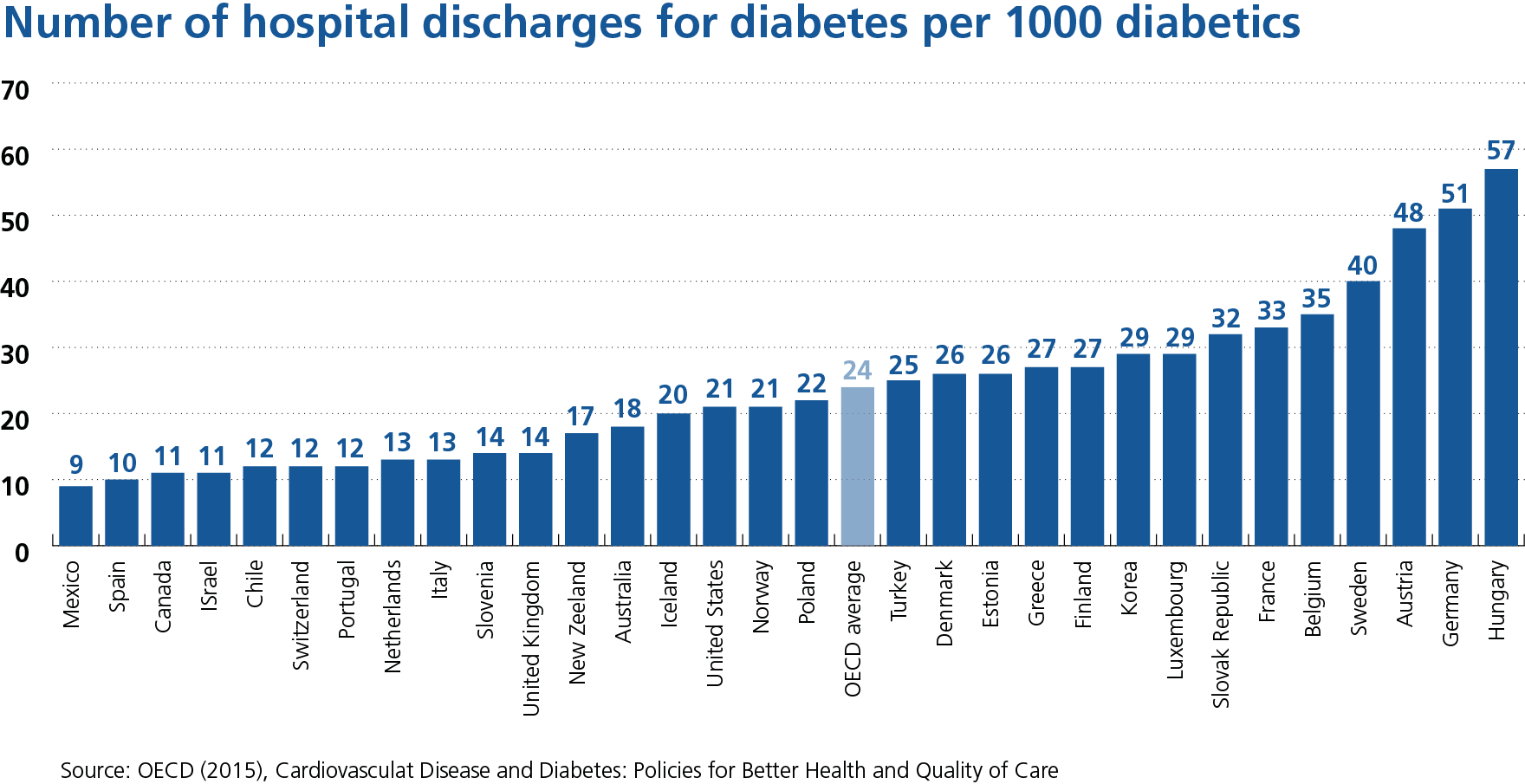
On average, 30% of health systems expenditure is spent on inpatient care. However, hospital admissions for chronic conditions are often avoidable, as illustrated by the wide variation between countries in the frequency of hospital discharges among patients with diabetes.
“A significant share of health spending in OECD countries is at best ineffective and at worst, wasteful. Solutions exist.”
Further opportunities to improve efficiency are explored in the EFPIA publication ‘Strengthening health systems through smart spending’ and other publications [Errea et al. 2020].
EFPIA champions efficiency and value-based healthcare, together with patients and other health stakeholders – including the European Alliance for Value in Health.
The pharmaceutical industry is committed to increasing the value of its products and services by focusing on the patient and patient outcomes and to demonstrating how innovative therapies can often decrease costs and thereby improve efficiency elsewhere in the system.
EFPIA and its members are also actively involved in various public-private partnerships that aim to improve efficiency, for example through health literacy and adherence to medicines in GravitateHealth.
Many EFPIA members have also united with other key stakeholders to create All.Can – a platform dedicated to improving the efficiency of cancer care by focusing on what matters to patients.
Industry: partnering for greater efficiency
Case study
Fostering LEAN methodology within Healthcare
Efficiency benefits the planet
Furthermore, it has been well documented that climate change can adversely impact human health. Its influence on health may be directly or indirectly from changing infectious disease patterns; increasing extreme weather events and the risk of drought, floods and subsequent food insecurity; and increasing respiratory disease from poor air quality. The recently published Commission Zero Pollution Action Plan, highlights the persistent threats of climate change, environmental pollution, biodiversity loss and an unsustainable use of natural resources which pose multiple risks to human, animal and ecosystem health. They include infectious and non-communicable diseases, antimicrobial resistance and water scarcity.
Europe is at the forefront of global efforts to reduce greenhouse gas emissions, with increasingly ambitious decarbonisation targets and various policy initiatives underway at EU and national level. In this context there is increasing attention on reducing the environmental footprint of health systems.
Efficiency is key to sustainability
We support the World Health Organization’s vision for an environmentally sustainable health system that improves, maintains or restores health while minimising negative impacts on the environment and leveraging opportunities to restore and improve it, to the benefit of the health and wellbeing of current and future generations. Furthermore, we welcomed and embraced the Commission’s focus on the Green Deal Strategy and a more sustainable Europe.
Like others, we believe that efforts to reduce the environmental impact of healthcare must not occur at the expense of health quality or equity. Rather, it will be best achieved by reducing unnecessary healthcare demand and consumption – as well as the impact of healthcare supply itself.
Therefore we agree with WHO and others that prioritising and incentivising disease prevention, improving chronic disease management, strengthening primary care, promoting innovative care models (including telemedicine) are key to improving the environmental sustainability of health systems, as well as their economic sustainability. In this respect, what’s good for patients and health systems is also good for the planet.
Pharmaceuticals in the environment
One of the unintended but inevitable results of delivering life-changing medicines to patients is that trace amounts of active pharmaceutical ingredients can find their way into the environment at all stages of the product’s lifecycle. The European pharmaceutical industry, represented by Association of the European Self-Care Industry (AESGP), EFPIA and Medicines for Europe is committed to continue playing an active role in addressing concerns around risks associated with pharmaceuticals in the environment. Minimising the impact of medicines on the environment while safeguarding access to effective treatments for patients is a critical issue across all sectors of healthcare.
We strive to contribute to a healthy environment and to lead efforts to mitigate climate change and the move towards circularity, in alignment with the aims of EU Green Deal and climate policy and circular economy vehicles. To this end we aim to deliver innovation that improves health outcomes while optimising resource consumption, supporting climate action.
Our commitment and action
In 2020 we published a White Paper on Climate Change, in which EFPIA members committed to:
- Establish climate change policies and strategies based on materiality and impact for individual companies, addressing their entire value chains (where the majority of emissions occur)
- Pursue science-based CO2 reduction targets and to annually and publicly disclose CO2 performance calculated according to recognised methodologies (e.g. the Greenhouse Gas Protocol)
- Contribute to reduced energy consumption and increased energy efficiency, and seek opportunities to use energy from renewable sources throughout the value chain .
Our Climate Change White Paper highlighted many examples of how EFPIA members are already reducing CO2 emissions and switching to alternative energy sources at company sites, and improving sustainability throughout their global supply chains. Furthermore, our Circular Economy White Paper provides examples of how companies are designing out waste and pollution, keeping products and materials in use and regenerating natural systems.
Multiple initiatives under the Eco-Pharmaco-Stewardship (EPS) have contributed over the last couple of years to improving scientific understanding, finding new ways to detect the trace amounts of pharmaceuticals in the environment, understanding their impact, prioritising active pharmaceutical ingredients posing a potential risk to the environment and also further reducing discharges from manufacturing plants. As an industry, we are striving to continually enhance our processes to deliver life-saving treatments in ways that are also protective of the environment.
These include the AMR Industry Alliance, which has developed a framework for assessing and promoting safe discharge targets for antibiotic manufacturing and the #medsdisposal campaign established to improve the collection of unused or expired medicines. Moreover, innovative risk-based frameworks such as our extended Environmental Risk Assessment (eERA) model and research initiatives such as IMI iPiE and IMI PREMIER recognise the importance of bringing different stakeholders together to address the ongoing concerns around pharmaceuticals in the environment.
References
European Alliance for Value in Health. Transforming towards value-based, sustainable, and people-centred health systems in Europe. 2020.
Available at https://www.europeanallianceforvalueinhealth.eu/wp-content/uploads/2020/11/EAVH-Transforming-European-Health-Systems-Feb-2021.pdf
https://www.europeanallianceforvalueinhealth.eu/value-based-health-systems/our-principles/
European Commission. Commission Green Deal Strategy December. European Commission, 2019. Available at https://ec.europa.eu/info/strategy/priorities-2019-2024/european-green-deal_en
European Commission. Zero Pollution Action Plan May 2021. European Commission, 2021.
Available at https://ec.europa.eu/environment/strategy/zero-pollution-action-plan_en
EFPIA. Value-based healthcare – an industry perspective. 2019.
Available at https://www.efpia.eu/media/412971/value-based-healthcare-an-industry-perspective.pdf
EFPIA. Strengthening health systems through smart spending. 2020.
Available at https://www.efpia.eu/news-events/the-efpia-view/statements-press-releases/strengthening-health-systems-through-smart-spending/
EFPIA. White paper on climate change. 2020.
Available at https://www.efpia.eu/media/554662/white-paper-climate-change.pdf
EFPIA Webpage on Environmental, Health, Safety and Sustainability. 2021.
Available at https://efpia.eu/about-medicines/development-of-medicines/regulations-safety-supply/environment-health-safety-and-sustainability/
EFPIA. White paper on Circular Economy. 2020.
Available at https://efpia.eu/media/554663/circular-economy.pdf
Errea M, et al. Opportunities to increase efficiency in healthcare. Office of Health Economics, 2020. Available at https://www.ohe.org/publications/opportunities-increase-efficiency-healthcare
European Academies Science Advisory Council; Federation of European Academies of Medicine. Decarbonisaiton of the health sector: a commentary by EASAC and FEAM. 2021.
Available at https://easac.eu/fileadmin/PDF_s/reports_statements/Health_Decarb/EASAC-FEAM_Decarbonisation_Health_Sector_Web_publication_FINAL.pdf
Eurostat. Preventable and treatable mortality statistics. 2020
https://ec.europa.eu/eurostat/statistics-explained/index.php/Preventable_and_treatable_mortality_statistics#Number_and_rate_of_avoidable_deaths
Faivre P, et al. Immunization funding across 28 European Countries. Expert Rev Vaccines 2021.
Epub Mar 24
GAVI. New evidence shows investments in vaccination produce even greater returns than previously thought. 2020. Available at https://www.gavi.org/vaccineswork/new-evidence-shows-investments-vaccination-produce-even-greater-returns-previously
Lenzen M, et al. The environmental footprint of health care: a global assessment.
Lancet Planet Health 2020;4:e271–79
OECD. Cardiovascular disease and diabetes: policies for better health and quality of care. OECD, 2015 Available at https://read.oecd-ilibrary.org/social-issues-migration-health/cardiovascular-disease-and-diabetes-policies-for-better-health-and-quality-of-care_9789264233010-en#page72
OECD. Tackling wasteful spending on health. OECD, 2017.
Available at https://www.oecd.org/health/tackling-wasteful-spending-on-health-9789264266414-en.htm
OECD. Health at a glance: Europe 2018. OECD, 2018.
Available at OECD. https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-europe-2018_health_glance_eur-2018-en
OECD. Health at a glance 2019: OECD indicators. OECD, 2019.
Available at https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2019_4dd50c09-en
OECD/European Union. Health at a Glance: Europe 2020: State of Health in the EU Cycle. OECD, 2020 https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-europe-2020_82129230-en?_ga=2.52510440.1357533625.1626362665-1150508910.1626362665
Ozawa S, et al. Return On Investment from childhood immunization in low- and middle-income countries, 2011-20. Health Aff (Millwood) 2016;35:199–20
WHO Regional Office for Europe. Environmentally sustainable health systems: a strategic document. WHO Regional Office for Europe, 2017. Available at https://apps.who.int/iris/handle/10665/340375