Industry remains committed to clinical trial data transparency
04.08.15
There is always a difference between advocating for change and delivering that change. Despite sharing the same aspiration, being responsible for delivery means careful consideration of the implications for patients and biopharmaceutical innovation; it requires investment in systems and processes as well as alignment to regulatory and legal frameworks. In that context, EFPIA and its member companies remain committed to working with stakeholders, and accountable to the Regulators, to ensure that clinical trial information is shared responsibly, taking into account patient anonymity, maintaining the integrity of regulatory systems worldwide and continuing to support innovation with appropriate arrangements for commercial-in-confidence information.
The article mentions the adoption of the EU Clinical Trial Regulation (536/2014) and publication of the EMA’s Transparency Policy (Policy 0070). To be clear, EFPIA and its member companies support the intent of the new regulation and are working actively with stakeholders such as the EMA to ensure its successful implementation. It is also worth noting that there is an existing mandatory EU requirement to register all interventional trials and disclose the summary results within 12 months of the end of the trial (within 6 months for paediatric trials) irrespective of the result. Every sponsor needs to adhere to these requirements.
However, industry progress on transparency is not limited to alignment with existing and new legislation.
Omitted from the Economist article, was the publication and subsequent implementation of the EFPIA/PhRMA Joint Principles for Responsible Clinical Trial Data Sharing (2014). Under this industry-led initiative, going beyond the requirements of the legislation, companies have been developing processes for access to patient level data from clinical trials. Typically, this means requests for patient level data are submitted by research organisations, the application is reviewed by an independent review panel or academic partner that makes the decision on granting access to the data and the data is then shared by the company. In the six months since implementation of the principles, an EFPIA survey of members revealed that 199 requests for data had been received: in 134 cases, data had been shared; 31 were rejected, with the remainder pending a decision at the time of the survey. There are case studies of this very real and tangible progress, turning principles into practice, available on the EFPIA website.
Principles for Responsible Clinical Trial Data Sharing
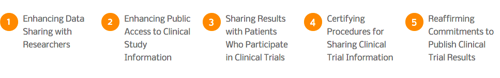
You can access more on the principles here.
As the article notes, much of the focus has been on developing systems for reporting current and future clinical trial information, however, we recognise there is also a demand from stakeholders for retrospective clinical trial data. Under the EFPIA/PhRMA principles, many companies are already making available data from retrospective studies.
Releasing retrospective data presents a number of significant challenges. Purely on a technical basis, retrieving older data sets and converting them to current data standards requires a substantial investment of resources. For example, it may be impossible to post retrospective data into current registries if there is missing administrative information. Another challenge is the resource required to ensure that retrospective data is reviewed to safeguard patient anonymity, and that commercially sensitive data remains confidential.
While not able to commit to systematically supplying older data, companies will, however, evaluate requests for older data on a case-by-case basis. In deciding to divert resource away from current research to releasing retrospective data, it is important to establish if the data is still clinically relevant or if there is more useful real world evidence on an existing product after years of its use in clinical practice.
The debate around clinical trial transparency, particularly the media coverage, has often been far too polarised. For me, the answer lies in collaboration: the entire research community needs to work together to strike a balance between sharing clinical data and protecting commercial-in-confidence information and patient anonymity. Patients across Europe need industry to continue to develop life-saving treatments, and the use of those treatments in clinical practice will be optimised by unfettered access to clinical data.
There is no transparency button lying idle in the basement of academic and industry scientific institutions. Organisations do not choose to flick a switch and disclose all data. It is a process of continuous learning and improvement, of developing systems and processes that work, and of listening to patients, clinicians, regulators, industry and academic researchers. This is the process in which EFPIA and its members, along with many others, are engaged, and to which they are committed.
