Trade policy and COVID-19: Openness and cooperation in times of a pandemic
01.04.20
Covid-19 has hit the world very hard in general and some regions so far in particular (e.g. China, Europe, US) over the past three months. The deep level of interconnectedness between countries and peoples across the globe, has allowed it to spread quickly globally after it originated in China, through overseas travels for business and holidays and within populations. As a response, countries are imposing measures to ‘flatten the curve’ in light of their health care system capacities and as advised by global and national experts. In doing so they are heavily constrained by the lack of necessary supplies (e.g. protective equipment, hand sanitisers, respirators).
Therefore, it is important to highlight how trade policy can help to fight the current pandemic. Trade measures could support the many national efforts that are currently ongoing to slow the spread of Covid-19 and to treat patients. However, according to Evenett (2020)[1], as of 21 March 2020, 46 export curbs on medical supplies were introduced by 54 governments since January this year, with most of them having been announced in March (See Figure 1).
Figure 1: Export curbs on medical supplies accelerated in March 2020
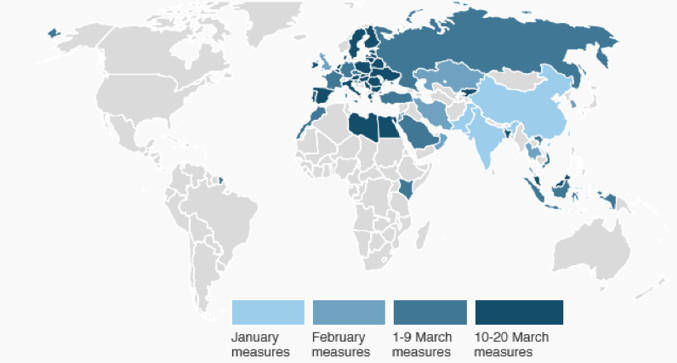
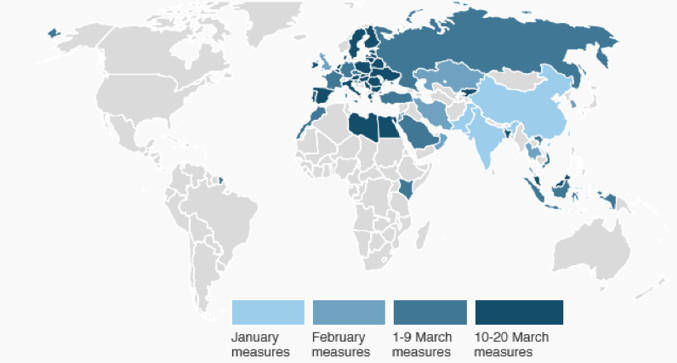
Source: Media reports, assembled by the Global Trade Alert Team, University of St. Gallen, Switzerland, 23 March 2020.
This is not the way to go as also highlighted in the March 30, 2020 G20 meeting. Trade restrictions amplify the lack of supplies, lead to inefficient distribution that will lead to loss of life, reduce the level of needed international coordination, and increase production problems in global value chains – in addition to the legal measures taken to combat the spread of Covid-19. The pharmaceutical and medical devices industries in particular are global industries. With their complicated global supply chains, they would be disproportionately impacted.
For example, Philips, one of the largest producers of ventilators in the world, used to produce a few thousand ventilators per month globally and now the demand is in the 100.000’s. The company has identified that in one machine there are 621 crucial components, all of which need to be ramped up if production of ventilators is to increase as well. This involves production facilities in many places globally, for example in the Philippines, where semi-finished products are produced. If that country is in lock-down, factory workers should still be able to go to their factory and work on these vital components otherwise global production for ventilators cannot be ramped up or even come to a halt. In addition, transport lines need to be kept going and the standards for all these parts and components need to be strictly adhered to (despite the pressure to ramp up production) to allow use of the devices at the ICs of hospitals.[2] The same risks we run for other essential supplies.
Trade measures should be focused on facilitating necessary supplies to healthcare workers and patients in need, as well as encourage developing new vaccines, medicines and diagnostics to treat Covid-19 in as short a timeframe as possible. They could be the following:
First, removing of tariffs on pharmaceutical products, medical devices and related medical supplies (e.g. protective equipment). Rather than closing markets or looking inwards for domestic production only, eliminating import tariffs on these goods will help our healthcare systems to continue to receive these critical supplies, produced by domestic and international producers. National governments across the globe should remove any tariffs on essential supplies unilaterally and the WTO-signatories to the zero-for-zero agreement could support by agreeing to extend this agreement that was last updated in 2010 to include all post-2010 intermediate chemical products, Active Pharmaceutical Ingredients (APIs) and final medicines – so they can cross borders tariff-free.
Second, removing or refraining from imposing export restrictions. It may at first glance appear intuitive to expect that imposing export restrictions will keep essential medical equipment in a country (and thus for policies to prioritize each national health service). In reality, globally integrated supply chains will be seriously disrupted, because national barriers cut through complex semi-finished and finished product systems, impact some supplies more than others, and prevent just-in-time management to operate. This will reduce supply globally. The 2006-2008 food crisis, for example, showed that export restrictions reduced global supply and caused significant price rises. Moreover, if one country puts export restrictions in place, others will follow suit. This would lead to fragmented availability in many countries and even no supplies to some countries. This applies also to relatively simple products like hand sanitizer. The EU sources 32% of its imports of medical supplies needed to fight Covid-19 from outside the EU. Finally, allocation of necessary equipment across countries could fail – leading to stocks in one country and patients dying in others.
Third, facilitating border-related trade of essential medicines and equipment. In spite of lockdowns in some countries and partial grounding of air fleets, it is essential that medicines and equipment continue to flow. Green (priority) lanes at borders for essential supplies or equivalent measures are crucial to avoid unnecessary delays. This would be particularly important so medicines with short shelf-lives would not go to waste. In addition, countries should be pragmatic with required documentation (e.g. import licenses) for essential supplies if their foreign representations (embassies) are closed and cannot provide the required documents any longer. Some evidence is emerging that due to the closing of embassies in some countries, necessary export documents can no longer be obtained leading to medicines and essential supplies being rejected from entry into (developing) countries, which could be detrimental.
Fourth, ensuring that all R&D and regulatory efforts – from the public and private sectors – are concentrated into developing vaccines, medicines and diagnostics against Covid-19. The appropriate intellectual property framework is enabling the rapid R&D response. Many potential treatments are based on decades of prior R&D and investment or originally were pioneered to treat other conditions. These breakthroughs were enabled by a robust innovation eco-system underpinned by effective IP. Within the Innovative Medicines Initiative (IMI) public-private partnership, a call to work together to develop medicines for Covid-19 and its symptoms and diagnostics for current and future outbreaks was launched and is under way. This complements the many other international efforts to develop vaccines at the same time. Currently around 20 vaccines are in the pipeline of being developed against Covid-19 and the hope is that in as little as 12-18 months a vaccine could be available (in comparison: developing a new vaccine normally takes between 10-15 years).[3] Current development ‘at pandemic speed’ can go faster if R&D steps are executed in parallel instead of sequentially (elevating financial risk)[4], can benefit from past experiences with and investments in vaccine development (e.g. SARS, MERS), and focused resourcing with all actors giving vaccine development the highest priority level. Trade can help to facilitate international collaboration and partnerships. The pharmaceutical industry is investing large sums of money to find a treatment and vaccine and has clarified it wants to work with governments and health systems to ensure that when these new treatments and vaccines are approved, they will be available and affordable. Regulatory authorities play a vital role in fast-tracking development of a new vaccine from a regulatory point of view, without jeopardizing quality and safety of patients (ICMRA, 2020).[5]
Fifth, ensuring the application of high regulatory standards to guarantee the quality and safety of imported essential supplies. Apart from tariffs, a lot of non-tariff measures constitute obstacles to global supply chains. The more global standards have already been developed across countries, the easier the quality of essential supplies can be maintained. For example, the existence of EU Mutual Recognition Agreements (MRAs) with countries on Good Manufacturing Practice (GMP) inspections now helps to keep a high production quality of globally shipped essential drugs. For other goods, this is harder. For example, for Personal Protective Equipment (PPE), standards differ globally. These differences in standards complicate international trade. The EU has eased conformity assessment rules for PPE to speed up the import of essential supplies at the moment.[6] Though this facilitates trade, there is also a related quality risk. For example, on March 28, in The Netherlands, it turned out that over 50% of the 1.3 million imported face masks from China did not meet the FFP-2 standard of protection and therefore could not be used.[7] To avoid countries wasting vital time and resources having to order new essential supplies to replace faulty ones standards must be upheld, even sometimes flexibilities can be introduced. No matter what we do to accelerate access to essential medicines and supplies, the quality, safety and efficacy of products cannot be compromised.
Sixth, allowing full and fast mobility of healthcare professionals and other essential personnel (e.g. factory workers in medicine production) across borders. This could include two measures. First, a temporary waiver regarding non-recognition of professional diploma’s for healthcare professionals (e.g. for doctors from China who have offered to advice and help in Europe). Second, a system to allow cross-border worker traffic for essential professions in order to avoid border restrictions like quarantine requirements from stopping them to move across (including for factory workers working on semi-finished and finished PPE and intermediate substances for medicines).
In order to beat the pandemic, we need global cooperation, sharing resources, and significant investments. The current increases in zero-sum unilateral trade policies could lead to tit-for-tat policies that hamper the global response to contain Covid-19. This could ultimately backfire, also for countries with sufficient supplies within their borders at this moment. European Commission for Trade, Mr. Phil Hogan, summarized the essence at the G20 meeting: “The COVID-19 pandemic is a global human tragedy, which requires a global collective response to protect human lives”.
[1] Evenett, S. (2020) ‘Tackling Covid-19 together – the Trade Policy dimension’, Global Trade Alert, March 2020.
[2] Interview with Mr. F. van Houten, CEO of Philips, Op 1, NPO 1, March 29, 2020.
[4] Lurie et al. (2020), Developing Covid-19 Vaccines at Pandemic Speed, New England Journal of Medicine, March 30, 2020.
